
Marissa Lawson, University of Washington and Christoph Lee, University of Washington
While mammograms are often the first step to detecting breast cancer, patients need additional tests after an abnormal screening result. Further imaging can determine if a finding is truly suspicious for cancer, and sometimes a biopsy is required to confirm a diagnosis. But biopsy delays reduce the benefit of early detection, putting patients at a higher risk of treatment failure and lowering their chances for survival.
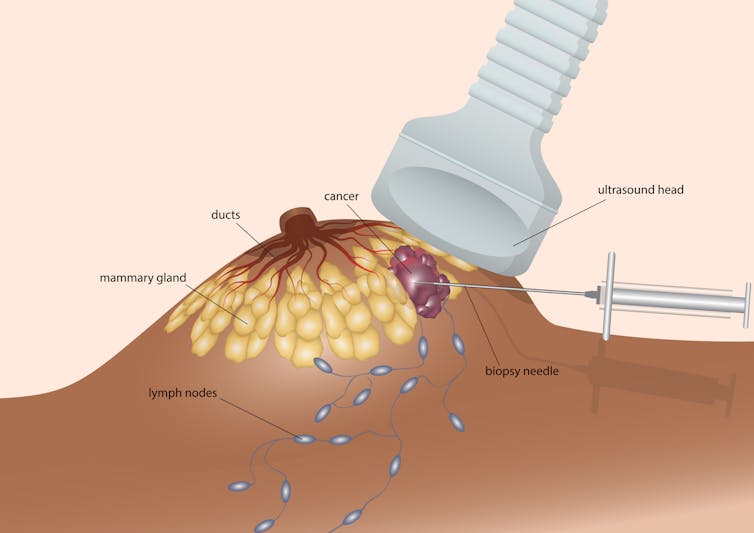
Breast biopsies involve removing a small piece of tissue from a suspicious area and examining the sample under a microscope. Once doctors are able to confirm the presence of tumor cells and what type they are, they are then able to devise a treatment plan.
Much prior research has looked at disparities in breast cancer care, including potential factors underlying diagnostic and treatment delays. On average, Black patients are more often diagnosed with late-stage breast cancer, have higher mortality rates and are less likely to receive guideline-recommended treatment compared with white patients. Hispanic and South Asian patients are also more often diagnosed with late-stage breast cancer compared with non-Hispanic white patients.
But previous studies have not looked at how multiple factors, including at the neighborhood and institutional level, can affect breast cancer care across diverse groups in different geographic locations. And not many studies have evaluated the disparities that may occur within the time-sensitive period between routine screening and an official diagnosis.
As radiologists who study health disparities and population health, we wanted to fill in this research gap. Our recently published study found that patients from racial and ethnic minority groups are more likely to have significant delays in getting a diagnosis-confirming breast biopsy after a mammogram compared with white patients.
Racial and ethnic differences in biopsy delays
We wanted to investigate potential reasons why some patients experienced a delay between when they received an abnormal mammogram result and when they underwent a diagnostic biopsy. So we used data from the Breast Cancer Surveillance Consortium, a network of imaging registries researching ways to improve breast cancer detection. We collected the demographic information of 45,186 patients in six states across the U.S. and analyzed their risk of not receiving a biopsy within 30, 60 or 90 days after getting an abnormal mammogram.
We found that all racial and ethnic minority groups experienced a higher risk of having a biopsy delay of over 30 days compared with white patients. Asian patients had the highest increased risk; they were 66% more likely to get a biopsy more than 30 days after their mammograms. When we looked at biopsy delays of 90 days or more, however, we found that only Black patients had a significantly increased risk – they were almost 30% more likely to experience extended delays compared with white patients.
Factors behind biopsy disparities
To figure out the potential reasons for these differences, we statistically accounted for other factors that may contribute to racial and ethnic differences in biopsy delays. These included individual-level factors, such as age and family history of breast cancer; neighborhood-level factors, such as area median income and education; and screening facility factors, such as academic affiliation and availability of on-site biopsy services.
We found that which screening facility a patient went to had the biggest effect on biopsy delays. This suggests that there are health care setting differences that could be contributing to longer wait times for nonwhite patients. These health care setting differences could include a number of factors, including whether there is a robust patient navigation system to provide guidance throughout the care process or the availability of same-day biopsies.
Our analysis suggests that nonwhite patients were still at higher risk of breast biopsy delays, even when we compared white and nonwhite patients with similar individual, neighborhood and screening facility characteristics.
This persistent difference in risks suggests that unmeasured factors such as structural racism, or ongoing policies and practices that lead to inequitable resource distribution for racial and ethnic minority communities, could also account for these differences. This could include health care coverage inequities with higher out-of-pocket costs, or policies that restrict access to higher quality care.
Structural racism may also have contributed to the facility-level disparities we saw. For example, facilities where more white people went to may have had additional resources allocated to patient navigators and same-day services that would have facilitated more timely biopsies.
Reducing the diagnostic gap
Long diagnostic delays after an abnormal screening mammogram can reduce the benefit of early cancer detection. Consequently, racial and ethnic differences in timely biopsy scheduling may exacerbate existing disparities in breast cancer diagnosis, treatment and survival – especially for Black patients.
While we were unable to identify more specific drivers behind these differences, we found that screening facilities do contribute to differences in biopsy delays among racial and ethnic groups. Our future work will focus on identifying facility-specific factors that may affect timely diagnosis after abnormal screening results. Our goal is to eventually be able to target these factors with interventions that reduce racial and ethnic disparities in breast cancer outcomes.![]()
Marissa Lawson, Medical Fellow in Radiology, School of Medicine, University of Washington and Christoph Lee, Professor of Radiology, School of Medicine, University of Washington
This article is republished from The Conversation under a Creative Commons license. Read the original article.
The views and opinions expressed in the article are solely those of their authors, and do not necessarily reflect the opinions and beliefs of AmericanScience.org.