Amanda Mascarelli, The Conversation
Heading into the third year of the COVID-19 pandemic, many of us have become amateur immunologists, having conversations at the dinner table and in the grocery store aisle about mRNA vaccines, variants, breakthrough infections, “waning” immunity, herd immunity, endemic viruses, booster shots and much more.
Many of the stories that we’ve published over the past two years here at The Conversation have stemmed from our own head-scratching questions that came up in our morning news meetings or were posed to us directly by curious readers. We sought out scholars who could take our readers on deep dives into immunology and virology to help demystify these sometimes confusing, conflicting and taxing science-based questions.
Here are five stories from The Conversation’s archives that highlight critical insights that we as editors and readers have gained thanks to COVID-19, and that will no doubt continue to be an important part of our pandemic lexicon.
1. COVID-19 vaccines explained
Understanding how vaccines can “trick” the body into mounting an effective immune response against a perceived or actual threat is one of the most fascinating aspects of immunology. “The most important thing to understand about vaccines is that they teach your body how to gear up to fight an infection, without your body having to deal with the infection itself,” writes Glenn J. Rapsinski, a pediatric infectious diseases fellow at the University of Pittsburgh Health Sciences. “In this way, vaccines help your body be prepared for invasions by germs that could otherwise make you very sick.”
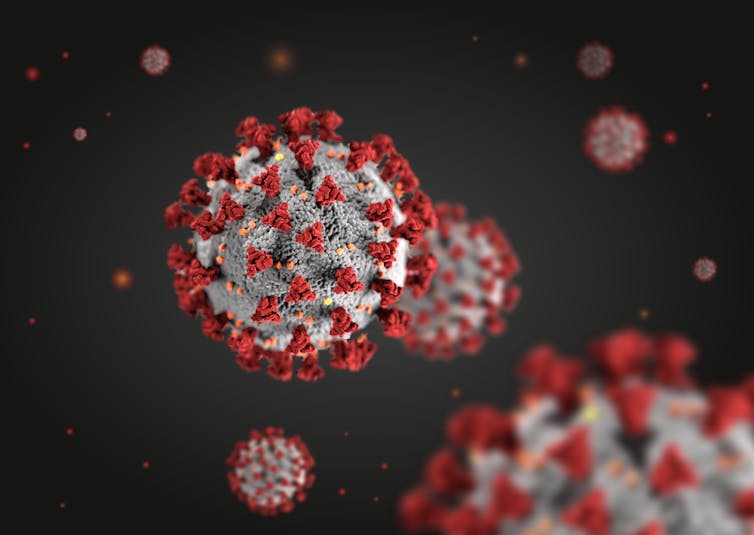
Rapsinski explains how the COVID-19 vaccines available in the U.S. emulate the spike protein of SARS-CoV-2, the virus that causes COVID-19. “SARS-CoV-2 is a round virus, with bumps all over it – sort of like a baseball covered in golf tees. The bumps are the spike proteins.”
2. And then came breakthrough infections
Soon after the relief that came with the widespread availability of vaccines in the spring of 2021, we were introduced to the idea of “breakthrough infections,” which were the rare cases in which fully vaccinated people got infected with COVID-19.
“Breakthrough infections are a little more frequent than previously expected and are probably increasing because of growing dominance of the delta variant,” Sanjay Mishra, a cancer and vaccine researcher from Vanderbilt University, wrote in July 2021. “But infections in vaccinated people are still very rare and usually cause mild or no symptoms.”
Although breakthrough infections became far more common late in 2021, in part because of the emergence of the highly transmissible omicron variant – more on that down below – COVID-19 vaccines still continue to provide robust protection against the most severe forms of COVID-19 that lead to hospitalization and death.
3. The growing list of variants
In 2020 and 2021, new strains of SARS-CoV-2 seemed to emerge faster than people could keep up with their Greek names. But by mid-2021, the highly transmissible delta variant had become the dominant strain in the U.S. and was responsible for the growing number of breakthrough infections. The continual emergence of variants was and is concerning, because it raises questions about how robust one’s immune protection will be from prior infections or from the COVID-19 vaccines, which were based on the original strain of the virus.
The delta variant was between 40% and 60% more transmissible than the alpha variant that it replaced and nearly twice as transmissible as the original SARS-CoV-2 virus, wrote Suresh V. Kuchipudi, a professor of emerging infectious diseases at Penn State.
But then, of course, came omicron, which was even more contagious than delta, thanks in part to its high number of mutations. “Omicron is very unusual in that it is by far the most heavily mutated variant yet of SARS-CoV-2, the virus that causes COVID-19,” Kuchipudi explained. “The omicron variant has 50 mutations overall, with 32 mutations on the spike protein alone. The spike protein – which forms protruding knobs on the outside of the SARS-CoV-2 virus – helps the virus adhere to cells so that it can gain entry.”
4. Putting ‘endemic’ viruses into context
At some point in 2021 – the year is one big blur – we entered a phase of the pandemic where it became clear that we were stuck with COVID-19 for the foreseeable future. For many people, there was a mental shift from the assumption that we could eradicate the coronavirus that causes COVID-19 through vaccination, into the slow realization that it just wasn’t going away. Virologists and other researchers began using the term “endemic” to describe the way that some viruses can fade away but still maintain a low level of transmission in a community.
Sara Sawyer, Arturo Barbachano-Guerrero and Cody Warren, a team of virologists and immunologists from the University of Colorado Boulder explain that SARS-CoV, the coronavirus that set off the SARS pandemic in 2003, was less contagious than SARS-CoV-2 and was brought under control relatively quickly by speedy public health measures that ultimately drove the virus extinct.
On the other hand, they wrote, “pandemic viruses may also gradually settle into a relatively stable rate of occurrence, maintaining a constant pool of infected hosts capable of spreading the virus to others.” Such viruses are said to be “endemic” – as will likely become the case with the coronavirus that causes COVID-19.
5. Immune defenses shift over time
As 2021 waned, so – apparently – did protective antibodies against COVID-19. Researchers began to learn more about how the immune response shifts in the months following COVID-19 infection or vaccination. And it became clear that over time, people became more vulnerable to getting reinfected or having a breakthrough infection following vaccination – in part because of the emergence of variants.
But antibodies are only part of the immune system’s protective defense, explain Prakash Nagarkatti and Mitzi Nagarkatti, a husband-and-wife team of immunologists from the University of South Carolina.
“Throughout the COVID-19 pandemic, the public has widely and mistakenly believed that antibodies provide the bulk of protective immunity, while not recognizing the important role of killer T cells,” they write. “This is in part because antibodies are easy to detect, whereas killer T-cell detection is complex and involves advanced technology. When antibodies fail, it is the killer T cells that are responsible for preventing the more severe outcomes of COVID-19, such as hospitalization and death.”
Editor’s note: This story is a roundup of articles from The Conversation’s archives.![]()
Amanda Mascarelli, Senior Health and Medicine Editor, The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
The views and opinions expressed in the article are solely those of their authors, and do not necessarily reflect the opinions and beliefs of AmericanScience.org.