Walter G. Johnson, Arizona State University and Diana Bowman, Arizona State University
The nomination of Judge Amy Coney Barrett to the U.S. Supreme Court has once again pushed the debate over when life begins into the headlines, which could have far-reaching effects on access to both current and emerging reproductive technologies. In 2006, Judge Barrett was one of the signatories on a newspaper ad sponsored by an anti-abortion group that not only believes life begins at fertilization but also hopes to criminalize discarding extra embryos created during in vitro fertilization.
As legal scholars, we are closely watching how jurisdictions regulate emerging reproductive technologies, including a set of techniques called mitochrondial replacement therapies which can prevent some heritable diseases. But because they use IVF methods, and some (but not all) of the techniques require discarding an embryo, law codifying the belief that life starts at fertilization could restrict access to mitochondrial replacement therapies and derail productive conversations about how to regulate them properly.
Implications for assisted reproduction
Last week, the medical journal Fertility & Sterility ran an editorial arguing that confirming Judge Barrett could result in restrictions not only on reproductive rights to contraception and abortion, but also on IVF. One concern is that future legal decisions could forbid IVF clinics from discarding extra embryos – even ones unlikely to start a pregnancy – or limit the number of embryos which can be formed. That could raise treatment costs or make efforts to start a healthy pregnancy with IVF much harder.
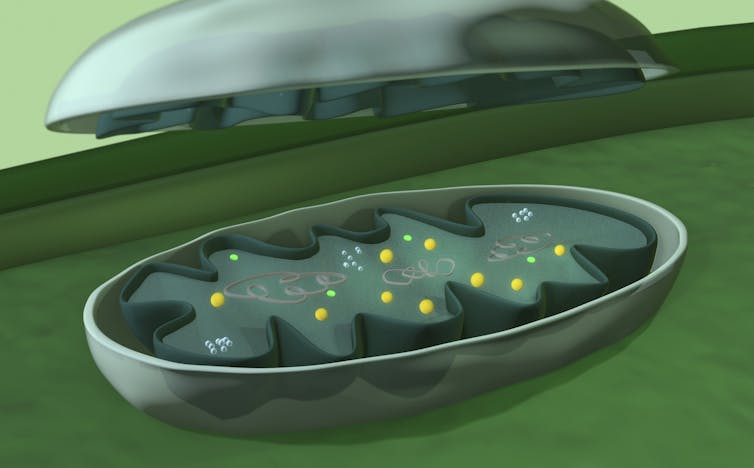
The nomination of Judge Barrett also comes just as new technologies look almost ready to help parents have children free of certain heritable diseases. Children can inherit mitochondrial diseases from their biological mother (and possibly their father) caused by dysfunctional mitochondria – which generate energy molecules for the cell. These tiny structures in the cell carry their own special DNA; but those that carry mutations can cause disease. A new type of reproductive technology called mitochondrial replacement therapies offers the possibility of preventing children from inheriting these diseases.
Mitochondrial replacement therapies
Estimates suggest 1,000-4,000 children in the U.S. alone are born each year with a heritable mitochondrial disease.
These complex diseases can affect many different organs – especially those with high energy needs like the brain, eyes or heart. There are no cures and few treatment options exist, so children often die in severe cases. Having a child with mitochondrial diseases can place huge emotional and financial tolls on families, with significant economic costs for health care systems.
With limited treatment options, some experts place more hope in preventing children from inheriting mitochondrial diseases altogether. Sometimes called “three parent IVF,” mitochondrial replacement therapies make this possible by replacing the unhealthy mitochondria in an egg cell or embryo with healthy ones from a donor woman. Using this technique, couples at high risk of having children with mitochondrial diseases can then have a healthy child who is biologically related to them.
Mitochondrial replacement therapies do, however, raise a few concerns. Health problems could arise from molecular mismatches between the parents’ nucleus and donor mitochondria or from a treated embryo reverting to an unhealthy state, though these risks are hypothetical for now. And female children born through mitochondrial replacement therapies could, theoretically, pass these conditions to their children.
Because mitochondria carry 37 of their own genes, children born from mitochondrial replacement therapies technically have DNA from three people – the couple and the woman who donated her healthy mitochondria. The donor contributes a minuscule amount of DNA – less than 1% – but this does raise questions about their “parenthood.” Another concern is that swapping out mitochondria (and their DNA) in embryos makes for a slippery slope to designer babies, especially now that three births have occurred after gene editing.
Regulating mitochondrial replacement therapies
These safety and ethical concerns call for policy to investigate and minimize risks, while answering questions like what the legal status of the third “parent” should be.
In 2015, the United Kingdom became the first jurisdiction in the world to expressly legalize and regulate mitochondrial replacement therapies, creating a system to license clinics for this service. This move came after an extensive public engagement process. Regulation is overseen by the Human Fertilisation and Embryology Authority, which governs all human fertility treatments and research within the U.K. Two other countries, Australia and Singapore, are considering legislative amendments to follow in the U.K.’s footsteps.
While brand-new regulatory systems for mitochondrial replacement therapies may seem ideal, lessons learned from other emerging technologies suggest most countries probably won’t adopt this approach – since existing rules often apply already, though maybe not in an ideal way. The trick then becomes making sure existing rules can still cover concerns with the new technology. However, this reality has led to critics raising the alarm about “unregulated” mitochondrial replacement therapies, especially since medical tourism is already happening.
Even if most countries don’t enact new laws, many already have rules which should apply to mitochondrial replacement therapies. For example, the U.S. won’t need a new regulatory system if it removes its current ban on the technology. The Food and Drug Administration already plans on regulating mitochondrial replacement therapies with the same tools it uses for “biologics,” a broad category of medical products ranging from vaccines to gene therapy.
Mexico got a bad reputation for having “no rules” after a child was born there via mitochondrial replacement therapies, but legal scholars have pointed out that Mexico’s regulations on health research likely prohibit this use of mitochondrial replacement therapies. However, these rules weren’t triggered because doctors modified the embryos in the U.S., before sending them to Guadalajara for the treatment. Instead, the U.S. FDA intervened, informing the clinic that they had violated U.S. law in several ways.
In Greece, regulators already approved a clinical trial for mitochondrial replacement therapies using their existing rules for fertility treatments – although the trial addresses the success of fertility treatments instead of preventing mitochondrial diseases. And in Ukraine, though the details are murky, health officials appear to have similarly approved a clinical trial for mitochondrial replacement therapies.
Moving forward
Reproductive technologies have allowed millions of families around the world to conceive healthy children over the last 42 years. For the first time, recent advances in mitochondrial replacement therapies could allow families who otherwise couldn’t have a healthy child of their own to do so. But changes in law that restrict access to IVF could have profound social and medical impacts that would ripple across the country.
[Deep knowledge, daily. Sign up for The Conversation’s newsletter.]
Rather than making reproductive technologies like mitochondrial replacement therapies more difficult to access – especially for those with a medical reason for doing so – we believe regulators and governments should be looking for ways to provide individuals access to these technologies in a way that promotes safety and efficacy for everyone involved. That includes those living in the U.S. who wish to access mitochondrial replacement therapies in their own country.![]()
Walter G. Johnson, Research Fellow, Arizona State University and Diana Bowman, Associate Dean for International Engagement in the College of Law, Arizona State University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
The views and opinions expressed in the article are solely those of their authors, and do not necessarily reflect the opinions and beliefs of AmericanScience.org.