Jennifer Doudna won the Nobel Prize for inventing a powerful gene editing technology. What comes next for CRISPR?
Written by Jina Moore Ngarambe
This article originally appeared inHarvard Public Health magazine. Subscribe to their newsletter.
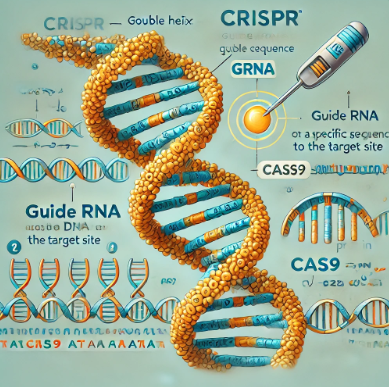
Among the things on Jennifer Doudna’s Nobel Prize-winning mind are cow farts. Cows' digestive processes release methane, and there are enough cows in the world that their natural gas is a major contributor to climate change. Doudna is working to genetically alter the microbiome of cows to produce less methane. It’s work made possible by the gene editing technology known as CRISPR, for which she shared the 2020 Nobel Prize in Chemistry. CRISPR uses a specific protein like a pair of scissors to splice genetic code, which Doudna describes as “a surgical tool at the molecular level”—one so precise, “we can alter a single letter of the DNA code in a cell.”
CRISPR now has dozens of approved and experimental applications. Besides making cows safer for the planet, Doudna’s also jazzed about bananas that never brown (now on sale in Japan), cattle without horns (not just yet), and innovations in research on Alzheimer’s and asthma.
And of course, there’s curing sickle cell anemia, perhaps CRISPR’s best-known application. Last year, the sickle cell treatment known as Casgevy became the first FDA-approved CRISPR therapy. “Who could have imagined that in just 10 years, we would get to an approved therapeutic with the very same molecule that we had studied academically?” Doudna says.
The speed of CRISPR’s development and the risks and ethical concerns raised by such technological advances were part of Doudna's conversation with Alice Park, TIME magazine’s senior health correspondent, at Aspen Ideas: Health, a three-day annual event in that idyllic town. Their hour-long discussion has been condensed and edited for Harvard Public Health by HPH editor Jina Moore Ngarambe.
Park: CRISPR is a double-edged sword. For scientists it's relatively easy, technology-wise, and it can be used for nefarious purposes. How did you initially think about unleashing this technology to the world, and how has your thinking around that changed?
Doudna: I remember being at a dinner at my house with some neighbors. One of them, a computer scientist . . . said, “Wait a minute, you mean you could put that in somebody's body and it could manipulate any of their genes?”
Not too long after that, a paper was published in a scientific journal in which a team reported that they were using CRISPR in monkey embryos to make germline changes, heritable changes, to DNA, and those edited embryos were implanted—monkeys were born with these heritable changes. And when I read that paper, I thought, “You know, there's no technical reason why this couldn't happen in humans.” And that was really for me that moment when I realized, okay, I have to get out of the lab and start talking about this because it's such a powerful tool. Humans now have a tool that can basically change who we are.
Park: You’ve talked about how, as a scientist, you didn't feel initially fully equipped to address those ethical, social, and cultural concerns. How did that change as the years went by?
Doudna: I definitely didn't. So I called two people [Paul Berg and David Baltimore] that actually had been at the forefront of an earlier iteration of ethical grappling in the 1970s, when the technology for manipulating bacteria came along. Scientists realized similarly that there could be real risk in manipulating the bacteria that populate our bodies, for example. Both of them were incredibly helpful in the CRISPR community and helping people like me to get our heads around what was coming with the technology, how to think about it, and how to initiate a more open discussion about it.
Park: And the things that they did around that technology, you modeled a lot of that around CRISPR—in terms of having a scientific community adopt a voluntary moratorium on certain applications of it in human embryos, for example.
Doudna: Right. I think that really started a whole movement in the field, in and among scientists, to get together and figure out how we were going to collectively manage a very powerful technology. We published a paper about it with the discussion of a moratorium, [and] we started being contacted by government agencies and regulators in different countries.
Park: Despite those best intentions, of course, in 2018, a Chinese scientist announced that he had actually done the worst case scenario and had used CRISPR to edit embryos that were then implanted, resulted in the birth of twin girls. Tell me about how you learned about that and the steps that you took immediately afterwards.
Doudna: I learned about that right before a conference that I was one of the co-organizers [of], that was being held in Hong Kong to discuss this very topic of human germline editing: Should we do it? How do we manage it? How do we control the technology? And this scientist got in touch and said, "Well, I've done this," and sent me a manuscript that he had drafted about the work.
He was already scheduled to speak at the conference, so our decision among the conference organizers was, let's have him come and present his work and open it up for questions.
It was a bit horrifying to hear what had been done. It really sounded unethical. There was an initial buzz around the work, but I think very quickly people realized that this isn't something that should be happening right now. The technology's not advanced enough to do it safely. And even if it was, we haven't had the opportunity as a community to figure out when and how should germline editing happen with something like CRISPR. That scientist was actually punished; he was ultimately jailed for that work. So that was like a real wake-up call.
Park: Currently the sickle cell treatment, as exciting as it is, I think the current price is about $2.2 million, which seems like a lot—but if you consider the kind of accrued cost of what patients pay throughout their lifetime for transfusions and other treatments, it could be a cost savings, ultimately. You're addressing this affordability issue and finding ways to also make it more accessible, especially in the clinical space. Can you tell us about some of the ways that CRISPR could potentially be[come] easier to do at more healthcare facilities, or for more providers to do?
Doudna: Well, let's start with what you said about CRISPR being a therapy that is kind of different than a traditional therapeutic. Because [for sickle cell] it's really a one-and-done treatment. When you give this treatment to patients once, they are effectively cured of their symptoms. And so if that is really true for something like sickle cell, you could argue that a price tag like the current one is, you know—maybe it actually makes financial sense when you look at the cost of care for patients over their lifetime.
On the other hand, it's a cost price point that absolutely won't work for the vast majority of people, both in this country and globally. And that's something that I think is not right. We need to address that. So we're working hard at our institute on ways to reduce the cost and make it much more affordable.
One of the big technical advances that we're working hard on [in an ongoing phase I clinical trial] is to make it possible to introduce the CRISPR molecules without requiring a bone marrow transplant for patients. That would make it much, much easier to give this therapy to people, and make it easier for manufacturing as well.
Park: [The sickle cell treatment] also requires chemo[therapy] now, right?
Doudna: Exactly, yeah. Which is also very invasive, and it's very unpleasant for patients. So I think there's a real opportunity, as exciting as it is to see this [current treatment], to make it even better.
Park: Looking ahead, what application of CRISPR are you most excited to see come into fruition?
Doudna: I'm really, really excited about this work we're doing [with] the microbiome. We're also working with a team at UC San Francisco where we're hoping to manipulate the human gut microbiome to reduce production of molecules that make children more susceptible to asthma. And if that approach works with asthma, you could imagine impacting the microbiome in other ways. We're just at the beginning of understanding how the microbiome affects our health in so many ways. And I think that having a technology that can allow us to manipulate that set of organisms that are so integral to our health is gonna be really powerful.
To hear Doudna discuss the rapidly growing agricultural uses of CRISPR, some early work toward using CRISPR for Alzheimer’s research, and her regrets about how intellectual property disputes have hampered some research, listen to the full conversation at Aspen Ideas: Health.