
Aging is a biological process that no one can avoid. Ideally, growing old should be a time to relax and enjoy the fruits of your labor. Aging also has a darker side, however, often linked to disease.
Every second, your cells perform billions of biochemical reactions that fuel essential functions for life, forming a highly interconnected metabolic network. This network enables cells to grow, proliferate and repair themselves, and its disruption can drive the aging process.
But does aging cause metabolic decline, or does metabolic disruption accelerate aging? Or both?
To address this chicken-or-egg question, you first need to understand how metabolic processes break down during aging and disease. I am a scientist and researcher, and my lab focuses on exploring the complex relationship between metabolism, stress and aging. Ultimately, we hope this work will provide strategies to promote healthier aging and more vibrant lives.
Link between metabolism and aging
Aging is the most significant risk factor for many of society’s most common diseases, including diabetes, cancer, cardiovascular disease and neurodegenerative disorders. A key factor behind the onset of these health issues is the disruption of cellular and metabolic homeostasis, or balance. Disrupting homeostasis destabilizes the body’s internal environment, leading to imbalances that can trigger a cascade of health issues, including metabolic disorders, chronic diseases and impaired cellular functions that contribute to aging and other serious conditions.
Disrupted metabolism is linked to many hallmarks of aging cells, such as telomere shortening, which is damage to the protective ends of chromosomes, and genomic instability, the tendency to form genetic mutations.
A dysfunctional metabolism is also linked to poorly functioning mitochondria; cellular senescence, or when cells stop dividing; imbalances in gut microbes; and cells’ reduced ability to detect and respond to different nutrients.
Neurological disorders, such as Alzheimer’s disease, are prime examples of age-related conditions with a strong link between dysregulated metabolism and functional decline. For example, my research team previously discovered that in aging mice, the ability of bone marrow cells to produce, store and use energy is suppressed due to increased activity from a protein that modulates inflammation. This energy-deficient state leads to an increase in inflammation that’s worsened by these aging cells’ reliance on glucose as their main fuel source.
Experimentally inhibiting this protein in the bone marrow cells of aging mice, however, revitalizes the cells’ ability to produce energy, reduces inflammation and improves plasticity of an area of the brain involved in memory. This finding suggests that some cognitive aging could be reversed by reprogramming the glucose metabolism of bone marrow cells to restore immune functions.
Repurposing drugs to treat Alzheimer’s
In our newly published research, my team and I discovered a new connection between disrupted glucose metabolism and neurodegenerative disease. This led us to identify a drug originally designed for cancer that could potentially be used to treat Alzheimer’s.
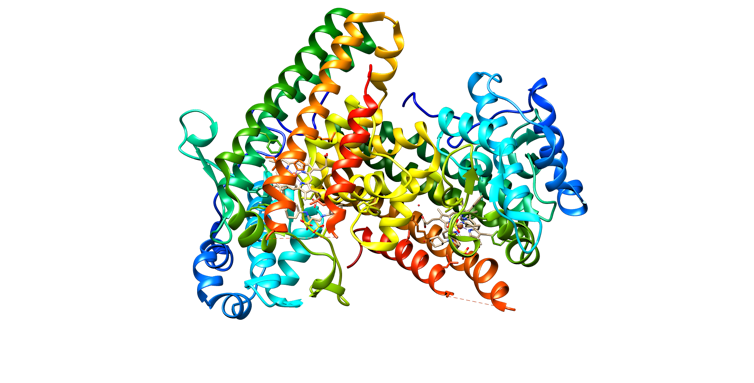
We focused on an enzyme called IDO1 that plays a critical role in the first step of breaking down amino acid tryptophan. This pathway produces a key compound called kynurenine, which fuels additional energy pathways and inflammatory responses. However, excessive kynurenine can have detrimental effects, including increasing the risk of developing Alzheimer’s.
We found that inhibiting IDO1 can recover memory and brain function in a range of preclinical models, including in cell cultures and mice. To understand why, we looked at the metabolism of brain cells. The brain is one of the most glucose-dependent tissues in the body. An inability to properly use glucose to fuel critical brain processes can lead to metabolic and cognitive decline.
High levels of IDO1 reduce glucose metabolism by producing excess kynurenine. So IDO1 inhibitors – originally designed to treat cancers such as melanoma, leukemia and breast cancer – could be repurposed to reduce kynurenine and improve brain function.
Using a range of lab models, including mice and cells from Alzheimer’s patients, we also found that IDO1 inhibitors can restore glucose metabolism in brain cells. Furthermore, we were able to restore glucose metabolism in mice with both amyloid and tau accumulation – abnormal proteins involved in many neurodegenerative disorders – by blocking IDO1. We believe repurposing these inhibitors could be beneficial across various neurodegenerative disorders.
Promoting healthier cognitive aging
The effects of neurological disorders and metabolic decline weigh heavily on individuals, families and the economy.
While many scientists have focused on targeting the downstream effects of these diseases, such as managing symptoms and slowing progression, treating these diseases earlier can improve cognition with aging. Our findings suggest that targeting metabolism has the potential to not only slow neurological decline but also to reverse the progression of neurodegenerative diseases such as Alzheimer’s, Parkinson’s and dementia.
Discovering new insights at the intersection of stress, metabolism and aging can pave the way for healthier aging. More research can improve our understanding of how metabolism affects stress responses and cellular balance throughout life.![]()
Melanie R. McReynolds, Assistant Professor of Biochemistry, Penn State
This article is republished from The Conversation under a Creative Commons license. Read the original article.